Outcomes of Hip Replacement
Total Hip replacement is listed as the 2nd most effective operation in terms of improving quality of life in the whole of surgery. The first is cataract surgery.
All of Mr Thomas’s patients are entered into the UK National Joint Registry.
His revision rate at 1 yr is very low at 0.7%
His infection rate is also extremely low at 0.3%
These figures are well below national averages.
Potential Complications of Hip Replacement
The majority of patients do extremely well after hip replacement surgery. It is an excellent operation for pain relief and restoration of movement and function. However complications can occur and delay recovery.
1. Infection – Incidence of deep infection is about 1%. This can mean prolonged antibiotics and even further surgery if it does not settle. Everything is done to minimise the risk with patients screened for MRSA pre-operatively, intravenous antibiotics at time of surgery and afterwards, surgery in a special laminar flow theatre and the surgeon wearing a “space suite” to minimise transmission of bacteria.
2. Thrombosis – Any surgery on the lower limb carries a risk of deep vein thrombosis and pulmonary embolus (clot in lung). There has been a lot of debate regarding giving patients medication to thin their blood preoperatively. Whilst in essence this sounds like a good idea, it can cause problems with bleeding during surgery and afterwards. This can then lead to a delay in recovery and an increased risk of infection. Mr Thomas therefore does not routinely give blood thinning agents apart from to those patients at high risk of thrombosis i.e previous clots, malignancy, blood disorders. The key to avoiding thrombosis is early mobilisation, so patients are asked to get out of bed as soon as possible after surgery. Mr Thomas uses foot pumps whilst patients are in bed and high dose Aspirin for 6 weeks. There is no definitive evidence in the literature as too what is best to use but this works well for Mr Thomas.
3. Dislocation – This is a specific risk to hip replacement and means that the hip can come out of joint with certain movements after surgery. In Mr Thomas’s practice, the risk is about 1-2% which is well below the national average. This comes down to surgeon technique and patient compliance post operatively.
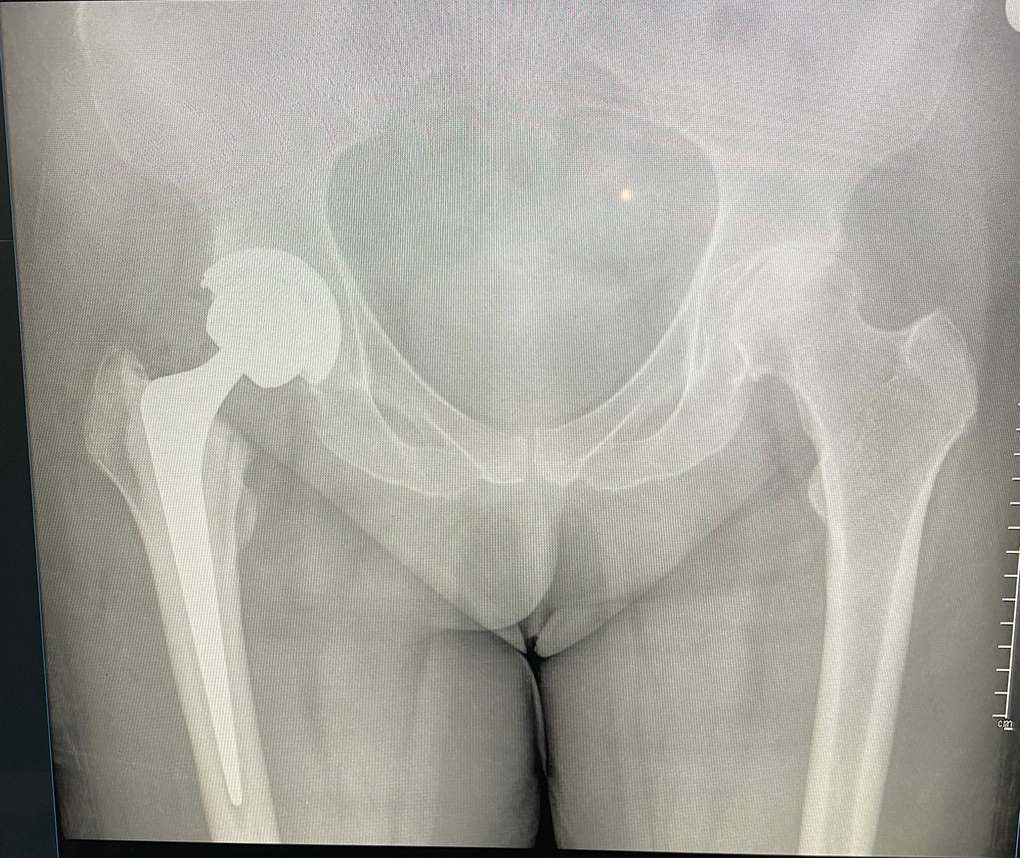
The use of larger femoral heads minimises this risk significantly.
4. Leg Length discrepancy – Mr Thomas strives to produce equal leg lengths. Computer software is used to template the surgery before
Post Operative Rehabilitation
The average length of stay in hospital is 2-3 days. Mr Thomas does operate on numerous young patients (under 50) with hip disease and this age group are often home at 2 days.
Patients are fully weight-bearing on their hip after surgery and may need crutches for up to 6 weeks afterwards. This is very variable amongst patients. Patients should have post operative physiotherapy to expedite recovery. If they are in a manual job, they will need at least 6 weeks off work. They should avoid driving for between 4 and 6 weeks.